EMP Guidance
National Emergency Medicine Report
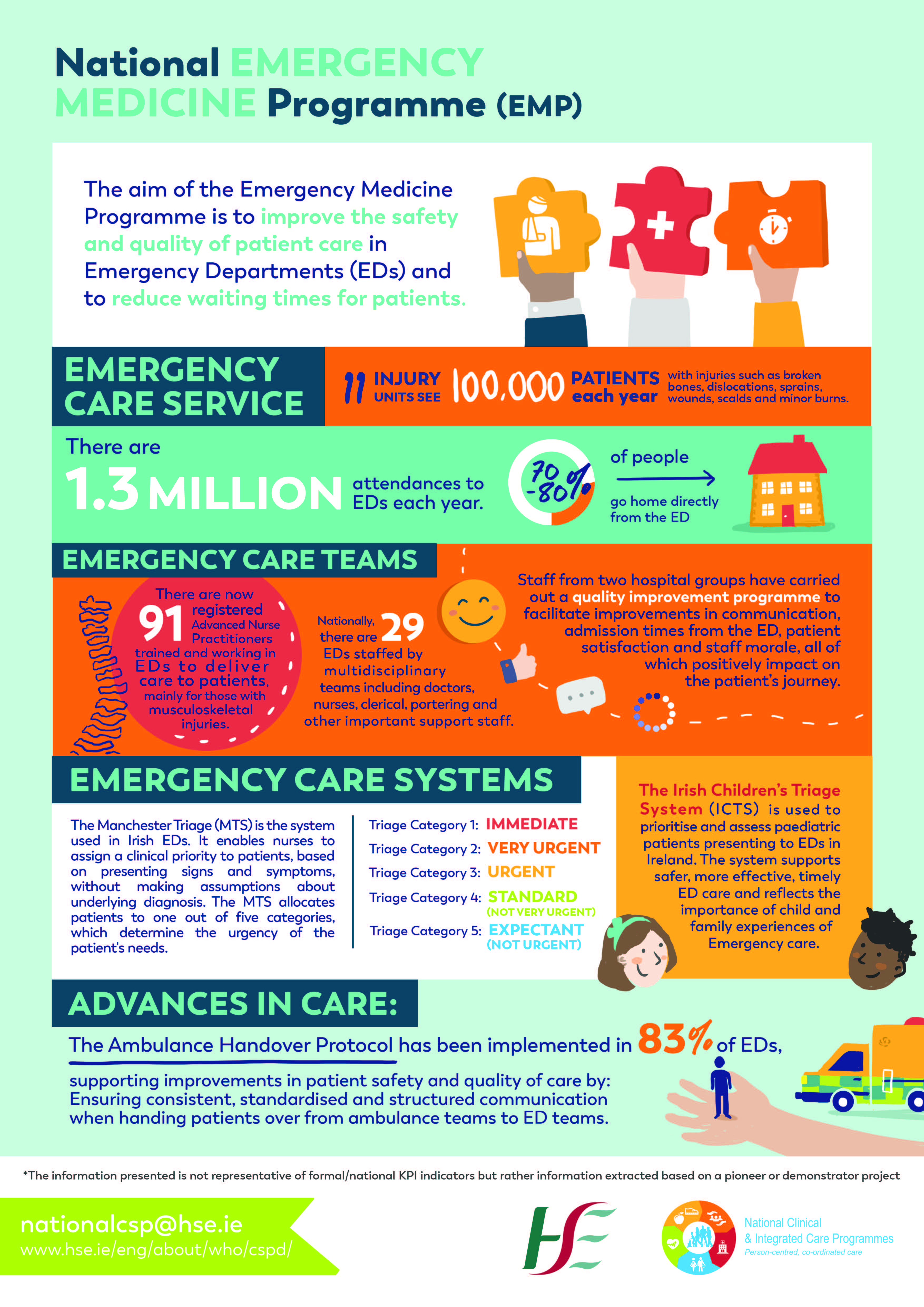
Understanding Emergency Care
Emergency medicine is a medical specialty — a field of practice based on the knowledge and skills required for the prevention, diagnosis and management of acute and urgent aspects of illness and injury affecting patients of all age groups with a full spectrum of undifferentiated physical and behavioural disorders. It further encompasses an understanding of the development of pre-hospital and in-hospital emergency medical systems and the skills necessary for this development.” International Federation for Emergency Medicine definition of Emergency Medicine.
An Emergency Department (ED) is a dedicated area in a hospital that is organised and administered to provide continuous access to Emergency Medicine (EM) services for patients and communities.
- EDs provide 24/7 access for undifferentiated emergency and urgent presentations across the entire spectrum of medical, surgical, trauma and behavioural conditions.
- Eds operate under the clinical governance of Consultants in EM. They are staffed by appropriately trained doctors, nurses and multidisciplinary healthcare provider teams.
- EDs require the on-site presence of core supporting specialties and services and must have seamless access to regional medical and surgical specialties and more complex diagnostic imaging facilities within an Emergency Care Network (ECN).
For more information on EDs and ECNs see Chapter 2, EMP Report 2012.
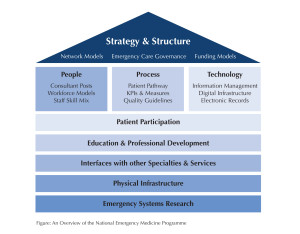
Emergency Care Networks, ECNs, are collaborating groups of Emergency Departments (EDs) and Injury Units (IUs) organised to deliver safe, high quality emergency care for local populations and communities. The aim of ECNs is to provide functional system networks that provide emergency care across the entire spectrum from high-acuity medical and surgical presentations, to complex psychosocial emergencies and non-life or limb threatening injuries. ECNs align the work of Pre-hospital and hospital-based emergency care services.
Core Emergency Medicine activities: • The prioritised evaluation and treatment of patients with time-critical and emergency health care needs; • The prioritised evaluation and treatment of patients with problems that are not immediately life-threatening or limb-threatening but which require emergency care to protect or restore the patient’s wellbeing or to prevent avoidable disability; • Essential supporting activities for clinical care and governance in EM; • Education, training and continuing professional development in EM; • Major Emergency planning. Valuable non-core Emergency Medicine activities: • Clinical Decision Unit – an inpatient facility adjacent to the ED managed by Consultants in Emergency Medicine; • Review clinic work; • Contributing to National Agencies and organisations relating to EM Service Development and Training. Important Emergency Medicine activities facilitated through specialist centres: • Research; • Medical Support for Pre-hospital Care.
HSE – The Emergency Department: How it works & what to expect – Currently being updated
HSE – Before you come to the Emergency Department – Currently being updated
Model of Care Guidance
Paediatric Emergency Care
Implementation of ICTS contributes significantly to paediatric patient care in our Emergency Departments and will promote safety, quality of care, improved access and patient experience in emergency care in Ireland.
Pre-Hospital Emergency Care
Pre-hospital Care (PHC) incorporates the primary response to injury and sudden illness, patient retrieval services, inter-hospital patient transfer, aspects of telemedicine and Major Emergency management and response. The delivery of PHC in Ireland is primarily the responsibility of the NATIONAL AMBULANCE SERVICE. DUBLIN FIRE BRIGADE provides an ambulance service in the Dublin area by agreement with the HSE NAS. The PRE-HOSPITAL EMERGENCY CARE COUNCIL is the statutory regulator for pre-hospital healthcare professionals. For further information on the role of Pre-hospital care in Emergency Care Networks please see CHAPTER 6 OF THE EMP REPORT 2012. CLICK HERE for information on the national protocol for the handover of care of patients transported by ambulance to EDs. – Reviewed in February 2021
Trauma Care
Trauma care involves Emergency Medicine, pre-hospital care, multiple medical and surgical specialties, healthcare organisations and other agencies and all have a contribution to make to the future development of trauma systems in Ireland. Trauma management involves all stages of the patient journey from pre-hospital care to rehabilitation and injury prevention. International research, education, audit and the development of trauma systems has resulted in improved outcomes for injured patients and has transformed the delivery of modern trauma care. The National Emergency Medicine Programme will work towards the establishment of Trauma Networks in conjunction with future acute hospital groups, Major Trauma Audit and a Trauma Registry in Ireland. The EMP has played a lead role in the development of the National Major Trauma Audit in the National Office for Clinical Audit. Please see Chapter 7 of the EMP Report 2012 for recommendations on the Organisation of Trauma Care in Ireland.
Major Emergency Planning